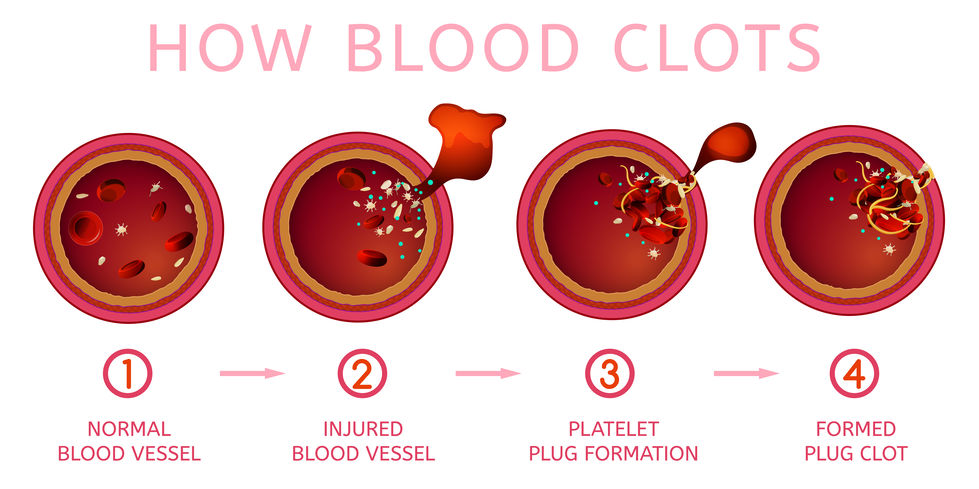
When your child scrapes their elbow or bruises their knee, blood vessels become broken, and blood escapes. The body responds quickly to prevent too much blood from escaping, using a process called blood clotting — when tiny cells in the blood clump together to fill small holes in the blood vessels that have been damaged.
Platelets are important cells that help the blood to clot. Without the right amount of platelets, your child’s body may not react to injuries as it should, putting them at risk for bleeding and bruising.
Immune Thrombocytopenia Purpura (ITP) is a bleeding disorder caused by the immune system. In ITP, the immune system makes antibodies that destroy platelets faster than the body can make them. This causes a low platelet count and puts your child at risk for bleeding and bruising.
Make An Appointment
Phone 402-955-3950 | Fax 402-955-3972
The exact cause of ITP is often unknown. However, ITP may develop after an illness or after
immunizations.
There are two different types of ITP:
- Acute ITP, which can last weeks to months
- Chronic ITP, which lasts longer than 12 months and can continue for several years
How Is Immune Thrombocytopenia Purpura Diagnosed?
In order to determine if your child has ITP, your child’s provider will perform a blood test to check their platelet count. If their platelet count is low, they may recommend more tests. One test that may be performed is a bone marrow aspiration. This test checks to see if your child’s bone marrow is making enough platelets.
Treating Immune Thrombocytopenia Purpura
Treatment is focused on decreasing your child’s risk of bleeding. Treatment may be different for
each child. Some children may only need one medication or treatment, while other children may need several. In some cases, ITP in children goes away without treatment.
When your child’s platelet count returns to normal without any medication or treatment, their ITP is resolved.
Initial treatment may include:
- Immunoglobulin (IVIG) is made from plasma and replaces the antibodies that are destroying platelets. This medication is given through the vein (IV).
- If your child is treated with IVIG, your child should wait 8 to 10 months after IVIG for live vaccines (MMR or varicella).
- Prednisone and Dexamethasone are steroids that help increase the platelet count. These medications are given by mouth or IV.
- Watchful waiting.
Secondary treatment may include:
- Rituximab (Rituxan®) is an antibody that decreases the immune cells that make antibodies against platelets. This medication is given through an IV.
- Romiplostim (Nplate®) helps increase the production of platelets. This medication is given as a subcutaneous injection (shot under the skin) every week.
- Eltrombopag (Promacta®) helps increase the production of platelets. This medication is taken by mouth daily.
- Anti-D (WinRho®) is made from plasma and has antibodies that attach to the red blood cells. Your child’s immune system then tells the body to get rid of red blood cells instead of the platelets. This causes the platelet count to increase, and red blood cell count to decrease (this is called anemia). This medication is given through an IV and can only be given to your child if their blood is Rh-positive, which means their blood contains the Rh antigen (a protein on the surface of their blood cells).
- Splenectomy (the spleen is surgically removed) may be considered for children with chronic ITP. The spleen’s job is to help your child’s body fight germs and infections, which means they may need to take antibiotics once it’s removed.
A platelet transfusion may be used as supportive care for severe bleeding. A platelet transfusion is a blood product given through an IV to temporarily increase the platelet count during treatment.
How To Prevent Complications From Immune Thrombocytopenia Purpura
If your child has ITP, it’s important to closely follow-up with your child’s hematologist for checkups and blood draws to monitor their platelet count.
Additionally, there are other guidelines you’ll need to follow to prevent bleeding:
- Do not give your child aspirin, Advil/Motrin (ibuprofen), or Naprosyn/Aleve (naproxen sodium).
- Your child should use a soft-bristled toothbrush when brushing their teeth.
The level of activity your child is able to participate in is based on their platelet count. If your child’s platelet count is:
- Greater than 50,000: They have no restrictions, but they need to avoid head injury and always wear a helmet when they’re riding a bike, scooter, or other similar equipment.
- 20,000 to 50,000: They cannot play contact sports or activities, ride a bike or scooter, or climb on jungle gyms, monkey bars, or any equipment they could fall from.
- Less than 20,000: They should only participate in quiet play, such as reading, drawing, coloring, watching TV, playing video games, or other activities with low risk of injury.
When To Seek Medical Attention
Call your child’s hematologist at 402-955-3950 right away if they have:
- Bruising
- Petechiae (tiny pinpoint red or purple spots on their skin)
- Blood in their urine or stools
- Bleeding gums
- Purpura (small red or purple spots on their skin)
- Bloody nose
Go to the Emergency Department right away if your child has:
- Headache
- Blurred vision
Additional Information On Immune Thrombocytopenia Purpura
For additional Information on ITP, visit:
What To Do Next
For Patients
To make an appointment, contact the Children’s Nebraska Hematology/Oncology Program at 402-955-3950.
For Referring Providers
The Physicians’ Priority Line is your 24-hour link to pediatric specialists at Children’s for referrals, emergency and urgent consults, physician-to-physician consults, admissions, and transport services. Call 855-850-KIDS (5437).
Learn more about referring patients.