
Discussing value-based care and alternative payment models requires becoming familiar with the topics’ lexicon. Here are explanations of some of the most common terminology in the value-based care and alternative payment model language:
Care Delivery
Accountable Care Organizations (ACOs)
Accountable Care Organizations are alliances of physicians, hospitals, and/or other health care providers that deliver and coordinate care for patients. The alliances may be formed through various structures, including but not limited to clinically integrated networks (CIN), independent practice associations (IPA), and physician-hospital organizations (PHO).
Care Coordination
Care coordination is management of referrals and information exchange among medical and non-medical professionals (e.g., “I need help managing multiple providers of care for my child with medical or social complexity.”)1
Care Management
Care management is the application of systems, science, incentives, and information to improve medical practice and help patients manage medical conditions more effectively (e.g., “I need help managing my child’s diabetes.”)2
Clinical Integration
Clinical integration is a vehicle through which providers are able to jointly contract directly with payers. It is a specific term that the Federal Trade Commission has defined as “an active and ongoing program to evaluate and modify practice patterns by the network’s physician participants and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality.”3
In summary, a clinically integrated network is a group of physicians organizing themselves to improve cost and quality by operating under a shared set of clinical guidelines and measures.
Independent Practice Association (IPA)
An independent physician association is a business entity organized and owned by a network of independent physician practices for the purpose of reducing overhead or pursuing business ventures such as contracts with employers, accountable care organizations and/or managed care organizations.
There are substantial opportunities for innovation in delivery system modeling and benefit design in the creation of physician networks. Specifically, creation of practice networks involving patient-centered medical home practices may accelerate important and necessary changes in health care delivery.4
Patient Attribution
Patient attribution is the method used to determine which provider or provider group is responsible for a patient’s care and costs.5
Most value-based arrangements are dependent upon a defined population of patients attributed to the contracting entity’s primary care providers (PCP). Although methodologies can vary (e.g., self-reported use of primary care, prescription data, select specialty care, etc.), they often use claims and encounter history to attribute the most relevant provider.
Patient-centered Medical Home (PCMH)
The Patient-centered Medical Home is a care model that transforms how primary care is organized and delivered. The Agency for Healthcare Research and Quality (AHRQ) defines a medical home not simply as a place but as a model of the organization of primary care that delivers the core functions of primary health care and encompasses the following five functions and attributes:
- Comprehensive care
- Patient-centered
- Coordinated care
- Accessible services
- Quality and safety.6
Patient-centered Medical Homes are delivery systems, not reimbursement models, that can be applied to and support provider performance within value-based care contracts.
Physician-Hospital Organization (PHO)
A physician-hospital organization is a legal entity generally formed by physicians and one or more hospitals with the intention of negotiating contracts with payers and sharing in the financial rewards of controlling costs while delivering high quality care.7
Population Health
Population health is a cohesive, integrated and comprehensive approach to health considering the distribution of health outcomes within a population, the health determinants that influence the distribution of care, and the policies and interventions that impact and are impacted by the determinants.8
Population Health Management
Population health management is a broad term to describe the collection of activities, resources, and tools focused on delivering value-based care. Population health management supports the aggregation of patient data across the care continuum, the analysis of that data into a single, actionable patient record, and the actions through which care providers can improve both clinical and financial outcomes.9
Total Cost of Care (TCOC)
Total cost of care is a broad indicator of spending for a given population (i.e., payments from payer to provider organizations). TCOC includes all spending associated with caring for a defined population, including provider and facility fees, inpatient and ambulatory care, pharmacy, behavioral health, laboratory, imaging, and other ancillary services.10
Total cost of care may be defined for a particular contract to exclude select services (e.g., behavioral health, pharmaceutical).
Triple Aim
Triple Aim is a framework developed by the Institute for Healthcare Improvement that aims to simultaneously improve the patient experience of care, improve the health of populations, and reduce per capita costs of care.11
Payment Models
Alternative Payment Models
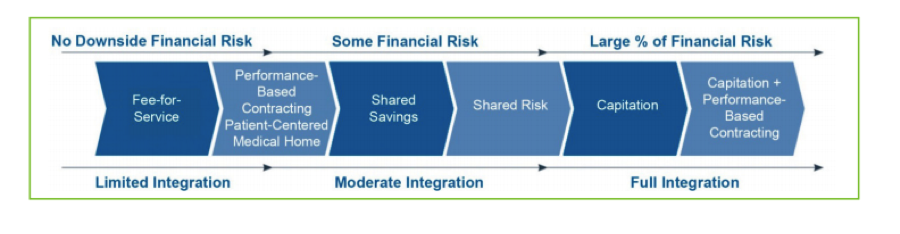
Alternative payment models are more advanced value-based contracting models where providers assume increased provider accountability for both quality and total cost of care, with a greater focus on the management of a population (e.g., shared savings, bundled payments, and capitation).12
The Health Care Payment Learning and Action Network, a national collaborative of providers, payers, employers, consumer groups and government agencies, has created an Alternative Payment Model Framework to measure, track, and use common terminology to support the transition from fee-for-service to alternative payment models.
| Category 1 | Category 2 | Category 3 | Category 4 |
|---|---|---|---|
| Fee for service: No link to quality and value | Fee for service: Link to quality and value | APMs built on fee-for-service archictecture | Population-based payment |
| A Foundational Payments for Infrastructure & Operations |
A APMs With Upside Gainsharing |
A Condition-Specific Population-Based Payment |
|
| B Pay for Reporting |
B APMs With Upside Gainsharing/Downside Risk |
||
| C Rewards for Performance |
|||
| D Rewards and Penalties for Performance |
Bundled Payments (e.g., Episode-based Payments)
A bundled payment is a reimbursement methodology with a fixed payment for all services associated with an episode of care. Bundled payments motivate providers to keep costs of care low while maintaining or improving quality. If costs exceed the fixed amount, the provider is held financially responsible for the difference (i.e., providers are not paid more). However, when clinical outcomes are good and the costs are kept low, providers are eligible to share in the financial gains.13
Capitated Payments (e.g., Population-based Payments, Global Payment)
Capitated payments are a reimbursement methodology where payments are paid on a per-member-per-month (PMPM) basis. Providers are paid a fixed-rate per member to cover a set of services for a specified population. Capitated payments are often made for all health care services but select services (e.g., behavioral health, pharmaceutical) may be carved out.
Providers assume full financial risk and are responsible for costs exceeding the fixed capitated amount but also receive full financial gains when costs are less than the fixed amount. In this model, providers accept full accountability for managing the total cost of care, quality, and outcomes for a defined patient population across the full continuum of care.14
Fee-for-service (FFS) Payments
Fee-for-service payments are a reimbursement system where providers are paid based on the volume of services delivered (e.g., visits, tests, treatments, procedures). In a FFS system, there is no incentive to prevent services with more effective coordination and management.15
Pay-For-Performance
Pay-for-performance is an incentive opportunity for providers to receive additional reimbursement for meeting defined quality and/or efficiency performance targets.
Pay-for-performance incentives are typically associated with existing fee-for-service contracts. Pay-for-performance is sometimes used as an umbrella term for initiatives aimed at improving the quality, efficiency, and overall value of health care.16
Shared Risk –Downside Risk
In a downside risk contract, providers share in the savings and potential losses. When the total cost of care is greater than the projected budgeted costs, providers are responsible for a defined percentage of the excess costs. Typically, providers assume downside risk for an opportunity for greater financial rewards (e.g., a higher defined percentage of shared savings).17
Upside Risk (e.g., Upside Gainsharing)
In an upside risk contract, providers share in the savings and not the risk of loss. When the total cost of care is lower than projected budgeted costs, providers receive a defined percentage of the difference between actual costs and budgeted costs (shared savings). However, if the actual total cost of care exceeds the projected budgeted cost, providers are not responsible for the difference.18
Upside Risk (e.g., Upside Gainsharing)
In an upside risk contract, providers share in the savings and not the risk of loss. When the total cost of care is lower than projected budgeted costs, providers receive a defined percentage of the difference between actual costs and budgeted costs (shared savings). However, if the actual total cost of care exceeds the projected budgeted cost, providers are not responsible for the difference.19
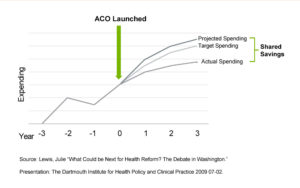
Shared Savings
Shared savings is a reimbursement methodology that evaluates providers on quality and cost of care. Shared savings contracts often include quality targets that must be achieved to be eligible for shared savings. When the actual total cost of care is lower than the projected budgeted cost of care, shared savings are achieved.
Providers receive a defined percentage of the savings as defined in the contract.9 Shared savings contracts give providers an opportunity to share in the savings they generate. In contrast, if savings were achieved within a fee-for service contract, all savings would accrue to the payer.
Value-based Care
Value-based care is a general term used to describe new payment models where providers are paid for keeping people healthy rather than the volume of services delivered. Value-based care arrangements can span from pay-for-performance contracts built on fee-for-service architecture to full capitation contracts with comprehensive population-based payments paid on a per-member-per-month basis.20
1 Adapted from Robert Mechanic. healthforum.brandeis.edu/about/staff-pages/mechanic.html.
2 Adapted from Robert Mechanic. healthforum.brandeis.edu/about/staff-pages/mechanic.html.
3 The 7 Components of a Clinical Integration Network. Becker’s Hospital Review. beckershospitalreview.com/hospital-physician-relationships/the-7-componentsof-a-clinical-integration-network.html. 8/01/2016.
4 Independent Physician Associations. American Academy of Family Physicians. aafp.org/about/policies/all/independent-physicianassoc.html.
5 Patient Attribution. Health Care Payment Learning & Action Network. June 30, 2016. hcp-lan.org/workproducts/pa-whitepaper-final.pdf.
6 Defining the PCMH. The Agency for Healthcare Research and Quality. pcmh.ahrq.gov/page/defining-pcmh. 7/31/2016.
7 Clinically Integrated Physician-Hospital Organizations. greatboards.org/newsletter/2009/Great-Boards-Winter-2009-reprint-Clinically-Integrated-PHOs.pdf
8 Nash, David B., et al. Population Health: Creating a Culture of Wellness. Sudbury, MA: Jones and Bartlett Learning, 2011. Print.
9 What is Population Health Management? Wellcentive. wellcentive.com/what-is-population-health-management. 8/1/2016.
10 Alternative Payment Models: Frequently Asked Questions. American Academy of Pediatrics. aap.org/en-us/professional-resources/practice-Transformation/Pages/ practice-transformation.aspx. 7/31/2016
11 Understanding Value-Based Healthcare. Moriates, C; Arora, V; Shah, N. 2015.
12 Alternative Payment Model Framework. Health Care Payment Learning and Action Network. January 12, 2016. hcp-lan.org/workproducts/apm-whitepaper.pdf.
13 The Payment Reform Landscape: Bundled Payment. Health Affairs Blog. July 2, 2014. healthaffairs.org/blog/2014/07/02/the-payment-reform-land.
14 Patient Attribution. Health Care Payment Learning & Action Network. June 30, 2016. hcp-lan.org/workproducts/pa-whitepaper-final.pdf.
15 Understanding Value-Based Healthcare. Moriates, C; Arora, V; Shah, N. 2015
16 Understanding Value-Based Healthcare. Moriates, C; Arora, V; Shah, N. 2015
17 Alternative Payment Models: Frequently Asked Questions. American Academy of Pediatrics. aap.org/en-us/professional-resources/practice-Transformation/Pages/ practice-transformation.aspx. 7/31/2016
18 Alternative Payment Models: Frequently Asked Questions. American Academy of Pediatrics. aap.org/en-us/professional-resources/practice-Transformation/Pages/ practice-transformation.aspx. 7/31/2016
19 Alternative Payment Models: Frequently Asked Questions. American Academy of Pediatrics. aap.org/en-us/professional-resources/practice-Transformation/Pages/ practice-transformation.aspx. 7/31/2016
20 Understanding Value-Based Healthcare. Moriates, C; Arora, V; Shah, N. 2015