When Jessica first laid eyes on her son, Jesse, he was the most beautiful baby in the world — but she knew he would face some challenges. Jesse was born with a bilateral cleft lip and palate, with a split in his upper lip and a palate (roof of mouth) that did not fuse properly during development.

“His facial anomalies never changed the way I felt about him,” said Jessica. “Jesse stole my heart from the moment he was born – all 9 pounds of him. He was precious and perfect in every way. When he made his grand debut on Aug. 1, 2020, I just couldn’t wait to be his mommy. I couldn’t wait to love on him and give him the best possible life any mother wants for their child.”
About 1 in every 1,600 babies is born with cleft lip and palate in the United States, according to the Centers for Disease Control and Prevention (CDC). If these conditions are left untreated, children may experience feeding and speech development difficulties, ear infections, hearing loss and dental problems. Luckily, the conditions can be treated with surgery.
One month after Jesse was born, Jessica was referred to Children’s Nebraska, where she met Dr. Oluwaseun Adetayo, Chief of Pediatric Plastic Surgery, for the first time. Dr. Adetayo discussed how she and the multidisciplinary craniofacial team would help restore function to Jesse’s lips and mouth, providing a more typical physical appearance.
“I was nervous about my baby going through his first surgery,” said Jessica. “But Dr. Adetayo had this way of calming my nerves and reassured me that everything would be okay. She broke things down in simple terms for me to understand and even drew helpful diagrams for me. Dr. Adetayo put all of my fears at ease and explained to me step-by-step how she would repair Jesse’s facial anomalies. From the moment I met her, I knew Jesse would be in good hands.”
Changing Jesse’s life, one surgery at a time

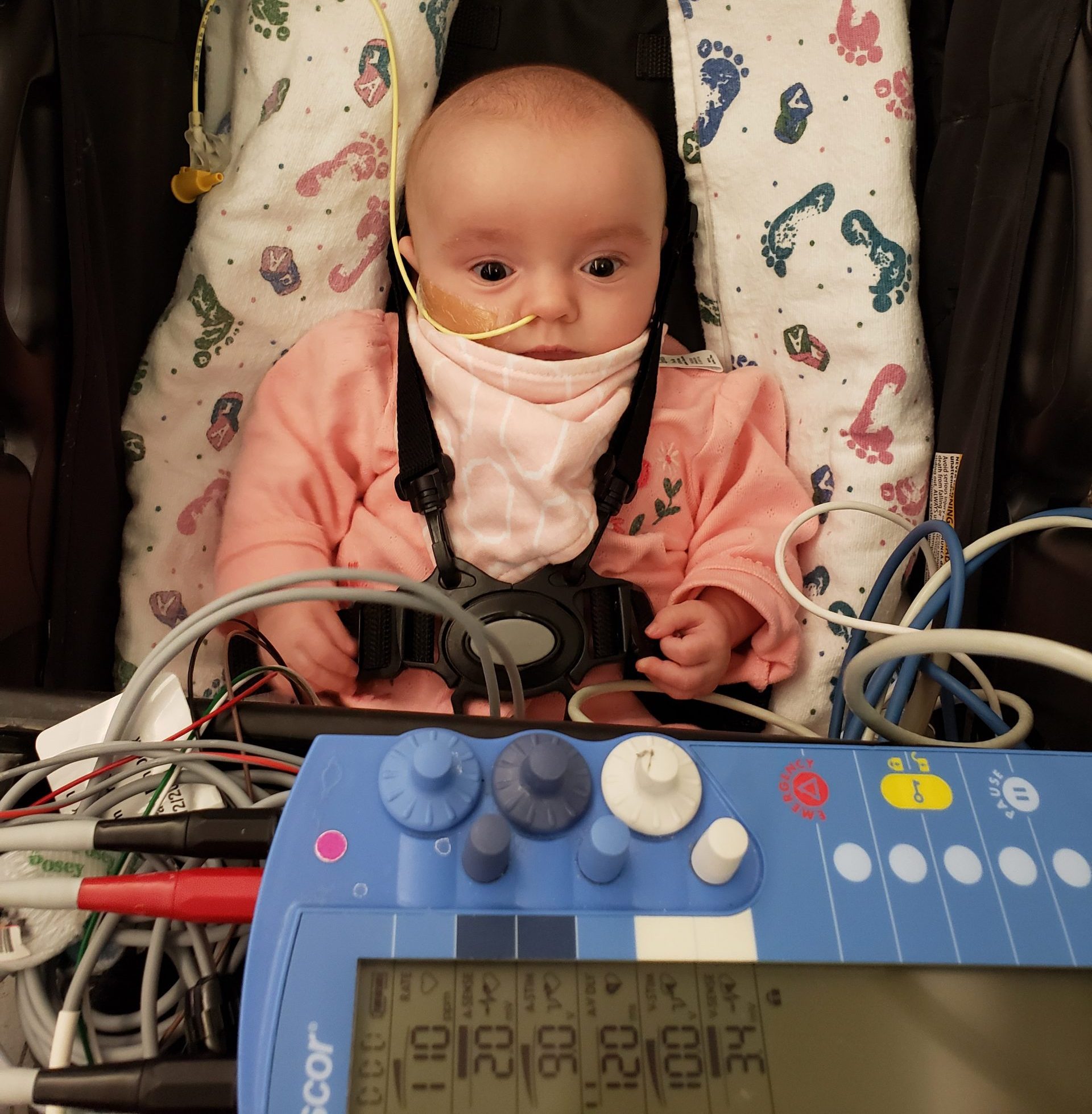
In December 2020, 4-month-old Jesse had surgery to correct his cleft lip. During this delicate procedure, Dr. Adetayo closed the opening in Jesse’s cleft lip and performed cleft rhinoplasty to reshape his nose so he could breathe better. Often, patients with a similar condition have an uneven nasal appearance due to their cleft lip and palate and need to undergo nasal reconstruction surgery.
“I was amazed when I saw Jesse after surgery,” said Jessica. “Dr. Adetayo and her team did a beautiful job. He looked different, and you couldn’t tell he had the deformity. Jesse spent a few days in the hospital until he was able to eat. Since he couldn’t suck because of his cleft palate, I fed Jesse with a big syringe.”
Shortly after celebrating his first birthday, Jesse was ready for his second surgery to repair his cleft palate. Cleft palate repairs are done when the child is older, between 9 months and 1 year old, to allow the palate to change as the baby grows and prevent further speech problems as the child develops. Dr. Adetayo also wanted Jesse to enjoy his first birthday cake and his favorite foods before his next surgery.
As with the first surgery, Dr. Adetayo drew a diagram for Jessica of what the surgery would look like before and after. In September 2021, Dr. Adetayo performed Jesse’s cleft palate repair. She closed the opening in the roof of his mouth, rearranged and repaired the muscles of the soft palate and made two incisions on each side of the palate to ease tension.
“Our plastic surgery team understands that birth anomalies can be difficult and overwhelming, especially when they are visible or affect a child’s development,” said Dr. Adetayo. “Our team is dedicated to helping children like Jesse function at their highest level. Jesse’s lip and palate repairs will improve his ability to eat, speak, hear and breathe. He can do the things now that any other child can do.”
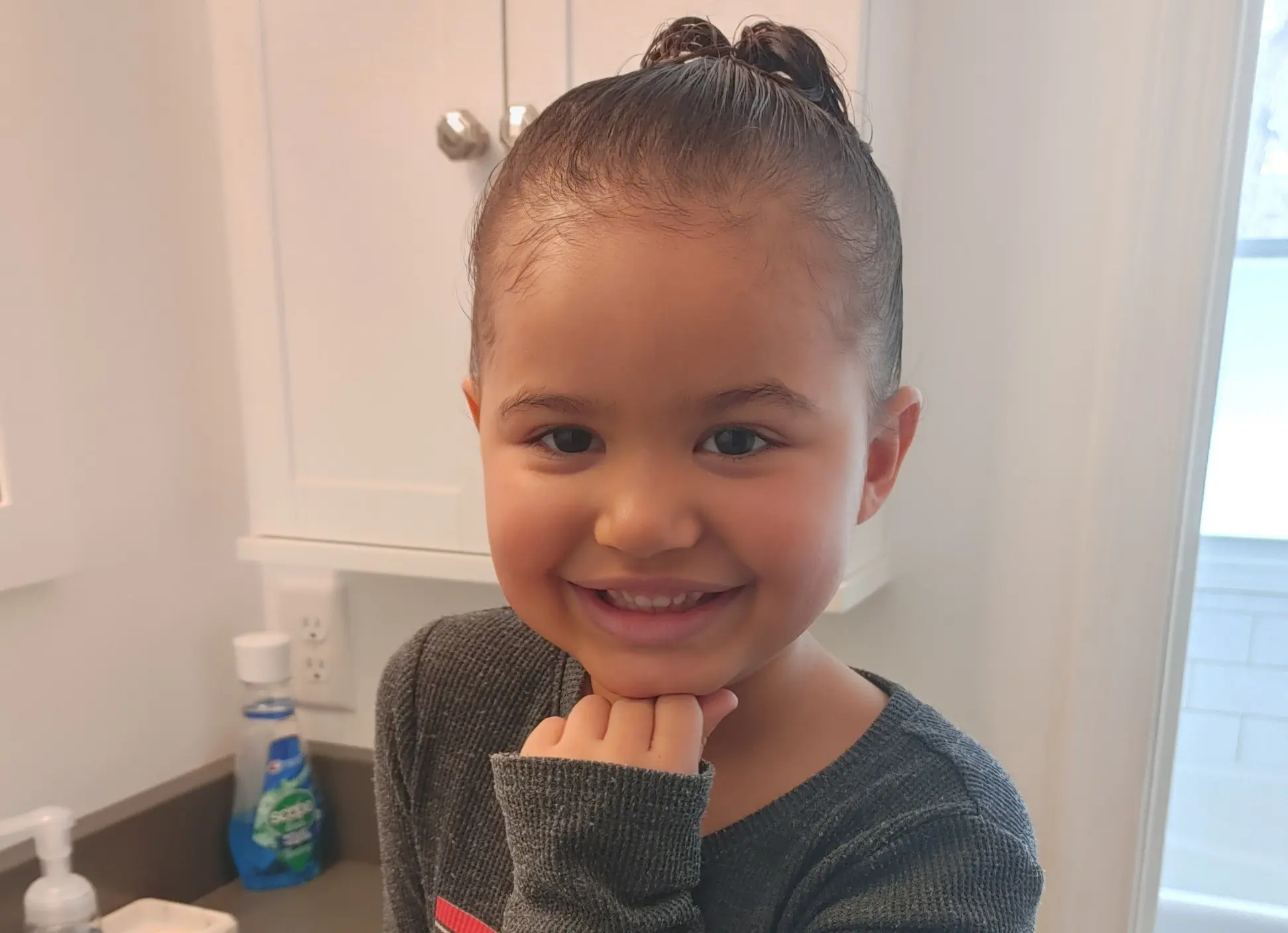
 To promote healing, Jesse had to wear arm splints to keep him from putting his fingers and sharp, pointy objects in his mouth, which could damage the sensitive tissues in his palate. Now that his palate has healed completely, Jesse is a happy baby who loves to eat and talk.
To promote healing, Jesse had to wear arm splints to keep him from putting his fingers and sharp, pointy objects in his mouth, which could damage the sensitive tissues in his palate. Now that his palate has healed completely, Jesse is a happy baby who loves to eat and talk.
“He is lovable and is the perfect addition to our family,” said Jessica. “He loves holding on to me and vies for all of my affection all the time. I wouldn’t have it any other way. His siblings adore him as well. While it has been a trying journey for our family, one thing that helped me a lot was joining support groups and engaging with other families of children with cleft lip and palate. It was great to share stories, listen to each other and have someone to lean on. I am thankful to Dr. Adetayo and her team for taking great care of Jesse and for the positive changes they made in my baby’s life. I see a bright future ahead of him.”
Click here to learn more about Children’s Plastic & Reconstructive Surgery team and the Craniofacial Center.
Plastic & Reconstructive Surgery
At Children’s Nebraska, we understand that birth defects or traumas can be difficult and overwhelming — especially when they are visible or affect a child’s development. Our specialists are here to help children ages 0 to 21 through all of their plastic surgery needs.